PCOS and Women’s Reproductive Health: What to Know
 Feb, 3 2026
Feb, 3 2026
One in ten women of reproductive age has PCOS. That’s more than 10 million women in the U.S. alone. Yet, most don’t know what it really means for their bodies - until they start missing periods, struggle to get pregnant, or notice sudden weight gain and acne that won’t go away. PCOS isn’t just about cysts on the ovaries. It’s a hormonal disorder that affects how your body makes and uses insulin, manages stress, and controls reproduction. And if you’re one of the women wondering why your body doesn’t work the way it "should," this is for you.
What Exactly Is PCOS?
PCOS stands for polycystic ovary syndrome. The name sounds scary, but the "cysts" aren’t tumors or dangerous growths. They’re small fluid-filled sacs - immature eggs that never got released during ovulation. The real problem isn’t the cysts. It’s the hormonal chaos behind them.
Women with PCOS typically have higher levels of androgens - male hormones like testosterone - than normal. This throws off the balance needed for regular ovulation. At the same time, many have insulin resistance. That means their bodies don’t respond well to insulin, the hormone that moves sugar from the blood into cells. The pancreas pumps out more insulin to compensate, which then pushes the ovaries to make even more testosterone. It’s a loop: high insulin → high testosterone → no ovulation → irregular periods.
It’s not genetic luck. It’s not just being overweight. It’s a mix of biology, environment, and lifestyle. And it shows up differently in every woman.
How PCOS Affects Reproductive Health
If you’re trying to get pregnant and it’s taking longer than expected, PCOS might be why. About 70-80% of women with PCOS have trouble ovulating regularly. That means fewer chances each month to conceive. Some women go months without a period. Others have bleeding that’s too heavy or too unpredictable.
But here’s the thing: having PCOS doesn’t mean you can’t get pregnant. It just means your path might look different. Many women with PCOS conceive naturally - especially when they manage insulin levels and body weight. Others need help from fertility treatments like clomiphene or letrozole. These medications help restart ovulation. IVF is also an option, but it’s not always necessary.
PCOS also raises the risk of pregnancy complications. Women with PCOS are more likely to have gestational diabetes, high blood pressure during pregnancy, and preterm birth. That’s why early care matters. If you’re trying to conceive, talk to your doctor before you get pregnant. Blood sugar, thyroid function, and hormone levels should be checked.
Other Signs You Might Have PCOS
Not everyone with PCOS has fertility issues. Some women don’t even realize they have it until they’re in their 30s or 40s. Here are the most common signs:
- Irregular or missing periods (fewer than eight per year)
- Excess facial or body hair (hirsutism)
- Severe acne on the face, chest, or back
- Thinning hair on the scalp (similar to male-pattern baldness)
- Weight gain, especially around the belly
- Dark patches of skin on the neck, armpits, or under the breasts
- Mood swings, anxiety, or depression
These symptoms don’t always show up together. One woman might have acne and hair growth but regular periods. Another might have weight gain and no visible signs at all. Diagnosis isn’t based on one symptom. It’s based on meeting at least two of three criteria: irregular ovulation, high androgen levels (confirmed by blood test), and polycystic ovaries on ultrasound.

How PCOS Changes Over Time
PCOS doesn’t go away after menopause. But the symptoms can shift. For example, the excess hair growth and acne often improve as estrogen levels drop. But insulin resistance doesn’t. That means the long-term risks - type 2 diabetes, heart disease, and high cholesterol - become more important.
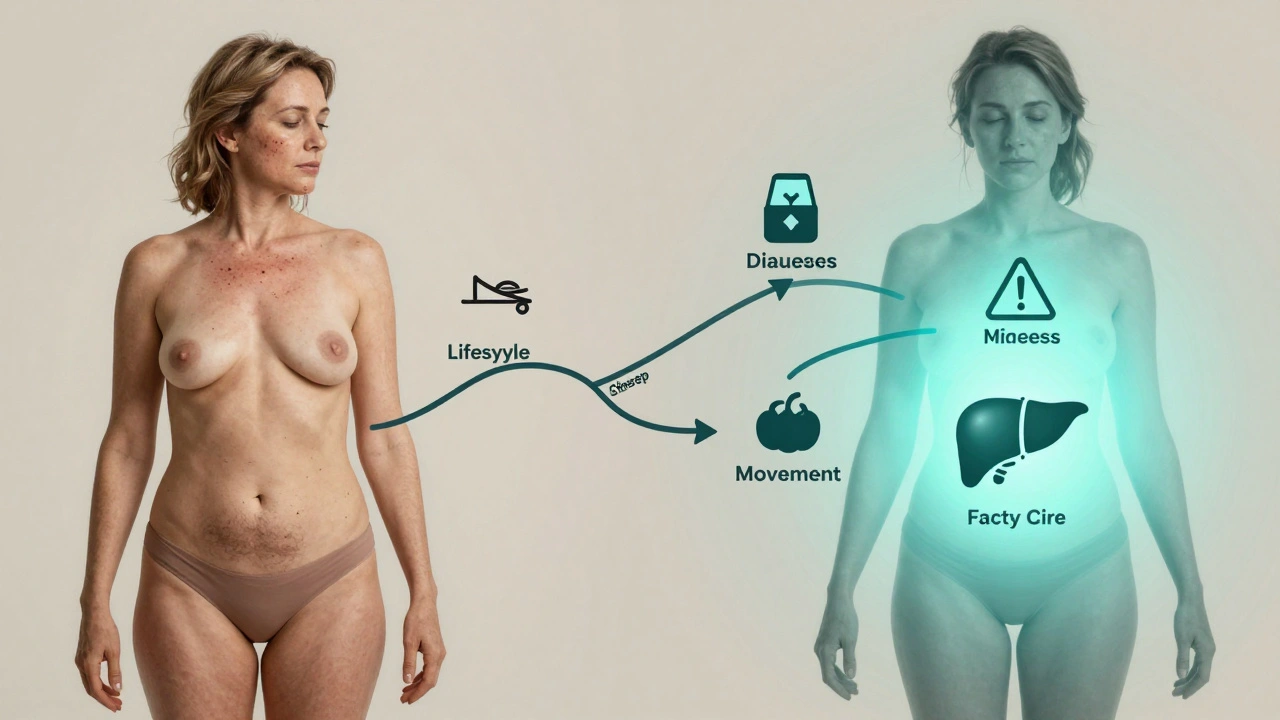
Women with PCOS are up to five times more likely to develop type 2 diabetes by age 40. They’re also at higher risk for sleep apnea, fatty liver disease, and endometrial cancer if periods are very infrequent for years. That’s why managing PCOS isn’t just about fertility. It’s about lifelong health.
What You Can Do: Lifestyle First
The most effective treatment for PCOS isn’t a pill. It’s food. Movement. Sleep. Stress management. Small, consistent changes make a bigger difference than any medication.
Studies show that losing just 5-10% of body weight can restore regular ovulation in many women with PCOS. That doesn’t mean starving yourself. It means eating more protein and fiber, cutting back on sugary drinks and refined carbs, and eating meals that stabilize blood sugar. Think eggs and spinach for breakfast. Lentils and broccoli for lunch. Grilled chicken with sweet potato and greens for dinner.
Exercise isn’t about burning calories. It’s about improving insulin sensitivity. You don’t need to run marathons. Thirty minutes of brisk walking five days a week helps. Strength training twice a week helps even more. Lifting weights builds muscle, and muscle uses glucose without needing insulin.
Sleep matters, too. Poor sleep raises cortisol, which worsens insulin resistance. Aim for seven to eight hours. Turn off screens an hour before bed. Keep your room cool. Stick to a bedtime, even on weekends.
And don’t ignore stress. Chronic stress spikes androgens. Yoga, deep breathing, journaling - even five minutes a day - can lower your body’s stress response over time.
Medications and Treatments
Lifestyle changes are the foundation. But sometimes, you need help.
- Birth control pills - These regulate periods, lower androgen levels, and reduce acne and hair growth. They don’t cure PCOS, but they help manage symptoms.
- Metformin - Originally for type 2 diabetes, this drug improves insulin sensitivity. Many women with PCOS see better ovulation and weight loss on it.
- Anti-androgens - Spironolactone can reduce facial hair and acne. It’s not safe during pregnancy, so birth control is usually prescribed with it.
- Fertility drugs - Clomiphene and letrozole are first-line treatments to trigger ovulation. Letrozole works better for women with PCOS in many cases.
Always talk to your doctor before starting anything. What works for one woman might not work for another.
When to See a Specialist
You don’t need to wait until you’re trying to get pregnant to get help. If you’ve had irregular periods for more than six months, or if you’re struggling with unexplained weight gain, acne, or hair growth, see a doctor. A gynecologist can start the conversation. But for complex cases, an endocrinologist or reproductive endocrinologist is often better.
Ask for blood tests: testosterone, LH, FSH, insulin, fasting glucose, and thyroid function. An ultrasound isn’t always needed - especially if symptoms are clear. But if you’re unsure, it can help confirm the diagnosis.
Breaking the Stigma
PCOS is often misunderstood. Some think it’s just "a weight problem." Others believe it’s all in your head. But it’s a real medical condition with real biological roots. It’s not your fault. It’s not laziness. It’s not failure.
And you’re not alone. Online communities, support groups, and doctors who specialize in PCOS are more common than ever. Find your people. Share your story. Ask questions. Your health matters - not just for fertility, but for your energy, your mood, your confidence, and your future.
What to Do Next
If you suspect you have PCOS:
- Track your periods for three months. Note when they start, how long they last, and how heavy they are.
- Write down symptoms: hair growth, acne, mood changes, energy levels.
- Make an appointment with your doctor. Bring your notes.
- Ask for blood tests: androgens, insulin, glucose, thyroid.
- Start with one lifestyle change: swap soda for water, take a 20-minute walk after dinner, or go to bed 30 minutes earlier.
Small steps lead to big changes. And you don’t need to fix everything at once.
Can you have PCOS and still have regular periods?
Yes. While irregular periods are a common sign, some women with PCOS have monthly cycles. But those cycles may not involve ovulation. You can have a period without releasing an egg. That’s why blood tests and symptoms matter more than just tracking your cycle.
Does PCOS mean I’ll never get pregnant?
No. Many women with PCOS get pregnant naturally. Others need help from fertility medications like letrozole or clomiphene. Even with insulin resistance, improving diet, movement, and sleep can restore ovulation. PCOS makes conception harder, but not impossible.
Is PCOS caused by being overweight?
No. While weight gain can worsen PCOS symptoms, many women with PCOS are at a normal weight or even thin. PCOS is rooted in hormonal and metabolic dysfunction, not body size. Insulin resistance and high androgens can happen regardless of weight.
Can diet alone manage PCOS?
Diet is one of the most powerful tools. Studies show that eating low-glycemic, high-fiber foods can improve insulin sensitivity and reduce androgen levels. Many women see improvements in ovulation, acne, and hair growth within 3-6 months of dietary changes. But combining diet with movement and sleep gives the best results.
Should I take metformin if I don’t have diabetes?
Yes - if your doctor recommends it. Metformin isn’t just for diabetes. It helps women with PCOS by lowering insulin levels, which can restore ovulation and reduce weight gain. It’s often prescribed even if blood sugar is normal, especially if other symptoms are severe.